CLINICAL: Thanks to long-acting antiretroviral therapy, which has changed lives of many living with the disease, according to a study…
By Kimberly McGhee
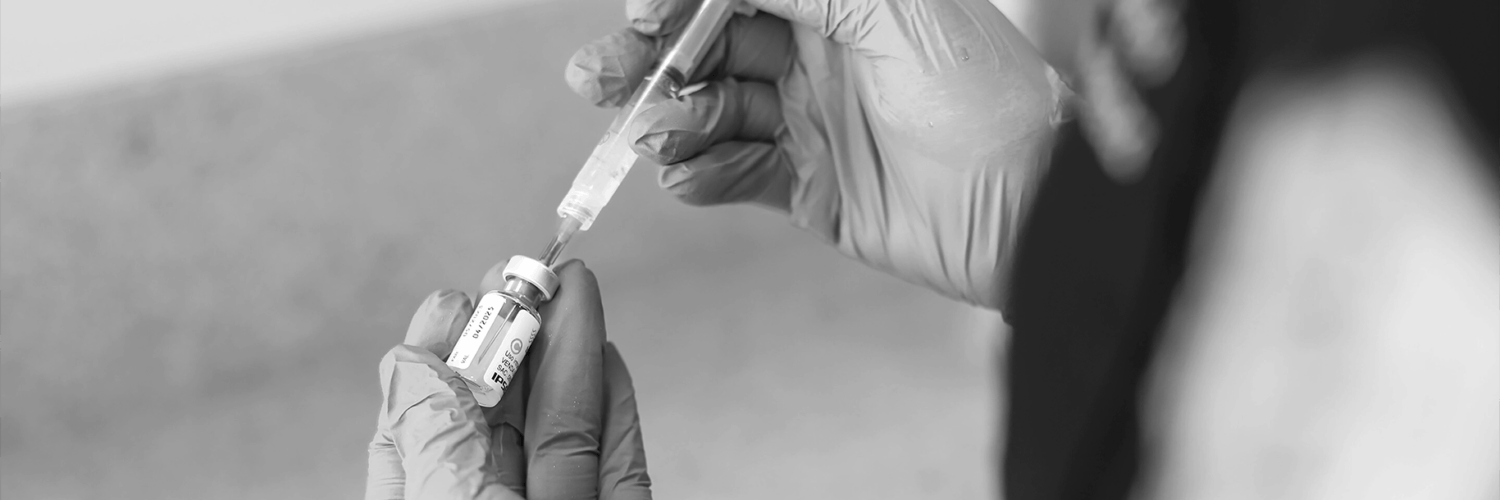
Long-acting injectable antiretroviral therapy (ART) can be administered at home to persons living with HIV as safely and effectively by a health care professional as in the clinic, with equally high patient satisfaction rates.
This is according to a new study conducted by Medical University of South California (MUSC) Health Infectious Diseases clinician Dr Eric Meissner, an associate professor in the College of Medicine. The findings of the study were published in Clinical Infectious Diseases.
“This project was designed at the time that injectable treatment for HIV infection received approval, and so we were inspired to try to think of new ways for the persons we care for to be able to access it,” said Meissner.
In the past three decades, ART has profoundly changed the lives of those living with HIV, transforming what was once considered a death sentence into something more akin to a manageable chronic disease. In 2023, almost 31 million people received ART, or about 77% of all people living with HIV.
Long-acting antiretrovirals are a class of medications designed to be administered less frequently than traditional daily oral antiretrovirals (ARVs), often on a monthly or bi-monthly basis, or even longer. They offer an alternative to daily pill-taking, which can improve adherence and improve treatment satisfaction for people living with HIV.
Currently, several ART brands are available for HIV-1 prevention and treatment, including cabotegravir, rilpivirine, lenacapavir, ibalizumab, and dapivirine.
Studies have shown that 9 in 10 people who take ART medications as prescribed will have undetectable levels of the virus within a year. People who achieve undetectable levels early in the course of their disease can live long lives, and they are unlikely to spread the virus to others, including unborn children. It is estimated that ART saves more than a million lives each year.
Unfortunately, in 2022, fewer than 65% of persons living with HIV in the United States achieved undetectable levels of the virus, according to the Centres for Disease Control and Prevention, suggesting that patients did not always take ART as directed. When orally administered, ART must be taken daily.
Some patients find it burdensome to take the medications daily or fear being stigmatized when they fill their prescriptions at a public pharmacy. Such barriers can discourage patients from taking the ART medications as their doctors suggest and can prevent them from attaining undetectable virus levels.
Long-acting injectable ART could be an answer, as it is given much more infrequently. Initially prescribed once monthly for persons living with HIV who did not gain full benefit from oral administration, long-acting injectable ART now need be administered only once every other month.
Studies have shown that these long-acting injectables make it more likely that patients will take medications as prescribed.
“For some people who struggle with daily pill medications for HIV, there have been studies showing that the injectable treatment does improve adherence and clinical outcomes,” said Meissner.
These injections must be given by a health care professional and are typically given when the patient is in the clinic. When long-acting injectables were approved for persons living with HIV who had not achieved undetectable limits with oral administration, Meissner took things a step further to determine whether long-acting injectables could be administered safely and effectively at home instead of in the clinic.
In Meissner’s study, 33 participants who had been prescribed long-acting injectable ART by their physicians were offered the choice of receiving the therapy in the MUSC Health Infectious Disease Clinic or at home. The South Carolina Clinical & Translational Research Institute provided regulatory and survey support for the study. Slightly more than half of participants (18) chose the clinic and 15 chose to receive their treatments at home. Participants were free to change their minds at any time and opt for the other treatment group.
The study found that, despite this freedom, most participants stuck with their original treatment choices. All patients in both groups who completed 12 months of treatment attained virological suppression.
Patient satisfaction scores were also very high for both groups, and no serious safety issues were observed for either group. More than half of participants experienced some temporary injection-site irritation, but there was no difference between the in-clinic and at-home groups.
For those choosing at-home therapy, Meissner and his team coordinated with the pharmacy to mail patients their medications, which were then stored in the refrigerator until the visit by the licensed practical nurse (LPN) who would give the injection. The same LPN administered long-acting injectable ART for all participants receiving therapy at home, and the study found high patient satisfaction with the continuity of care that this provided.
The study answered another of Meissner’s questions—what influenced participants to choose either the clinic or at home. The answer for both was the same: convenience.
“Convenience was far and away the most commonly stated reason driving the preference for where to receive treatment,” said Meissner. “I think that relates to the fact that a significant percentage of our cohort doesn’t live right next to our clinic. Many may have difficulty with the time and the logistics of transportation required to come to our downtown clinic.”
Despite the high patient satisfaction with at-home administration of long-acting injectables, it will be challenging to make this a routine option for persons living with HIV. Providing the medication by mail and scheduling the LPN visits required considerable logistical coordination by staff.
Currently, insurance or medical aid schemes do not reimburse for these additional steps, making it unlikely that physicians will be able to offer this option. If these challenges can be overcome, however, Meissner’s study suggests that many patients would benefit and appreciate the option, which could encourage them to follow the treatment course set out by their physicians.
“As to administering injectable HIV treatment in someone’s home, we found it to be safe, feasible and associated with high satisfaction for the people who elected to receive it there,” said Meissner. “And so I’m enthusiastic for continued systematic and infrastructure-based efforts to provide people with more choices about where to receive this treatment.”
ARTs are available in South Africa for both HIV prevention and treatment. For prevention, cabotegravir long-acting (CAB-LA) is an injectable PrEP option, and the dapivirine vaginal ring is also available. For treatment, while injectable cabotegravir and rilpivirine are approved for use in other regions, they are not yet available in South Africa due to registration and cost issue.
In 2022, the WHO recommended the innovative long-acting injectable version of HIV Pre-exposure Prophylaxis (PrEP), Cabotegravir (CAB-LA), as part of a comprehensive approach to HIV prevention. CAB-LA has been described as a potential game-changer in the fight against HIV, a disease that has affected many people. Nearly 40 million people were living with HIV at the end of 2023, while over 88 million have been infected since the beginning of the epidemic.
Four African countries started offering CAB-LA in 2024: Zimbabwe, Malawi, Zambia, and Eswatini in April. South Africa was scheduled to receive a portion of the 231 000 doses of CAB-LA from the President’s Emergency Plan for AIDS Relief (PEPFAR) anytime between October and December last year, and the remainder will be released over two years, according to Doctors Without Borders in November in a statement released in November last year.
The entity also announced it had successfully secured a limited number of doses of CAB-LA and is preparing for the initial rollout of projects across Zimbabwe, Mozambique, Malawi and Eswatini. – Tuft University and additional reporting by WSAM